MTIMA: Beginning. Blantyre, Where Training Turns Into Care.
On a warm morning in Blantyre, the ultrasound room at Queen Elizabeth Central Hospital hums at the pace of the city outside—minibuses threading Limbe, market stalls opening, the hills ringing with radios. A trainee steadies the probe; the screen sharpens from static to structure. Leaflets of a mitral valve appear, then measurements, then a plan. It’s a small scene with large consequences: skill taking root, owned locally, repeatable tomorrow.
MTIMA, a Canadian-registered NGO, builds its work around moments like this. The organization’s premise is straightforward and unfashionable in a world that rewards spectacle: the most durable gains in Malawian heart care will be led by Malawian clinicians. In Blantyre, that means working alongside teams at Queen Elizabeth Central Hospital and the Kamuzu University of Health Sciences—teaching, standardizing, and troubleshooting until precision becomes habit.
The stakes are not abstract. Cardiovascular disease is now a major share of Malawi’s non-communicable disease burden, a priority echoed in the country’s own policy documents and in global targets. In practical terms, that looks like shortness of breath that might be heart failure, a murmur that could be rheumatic valve disease, a chest pain case that needs triage today, not next week. The distance between suspicion and treatment is measured in images and decisions. MTIMA’s job is to make both clearer.
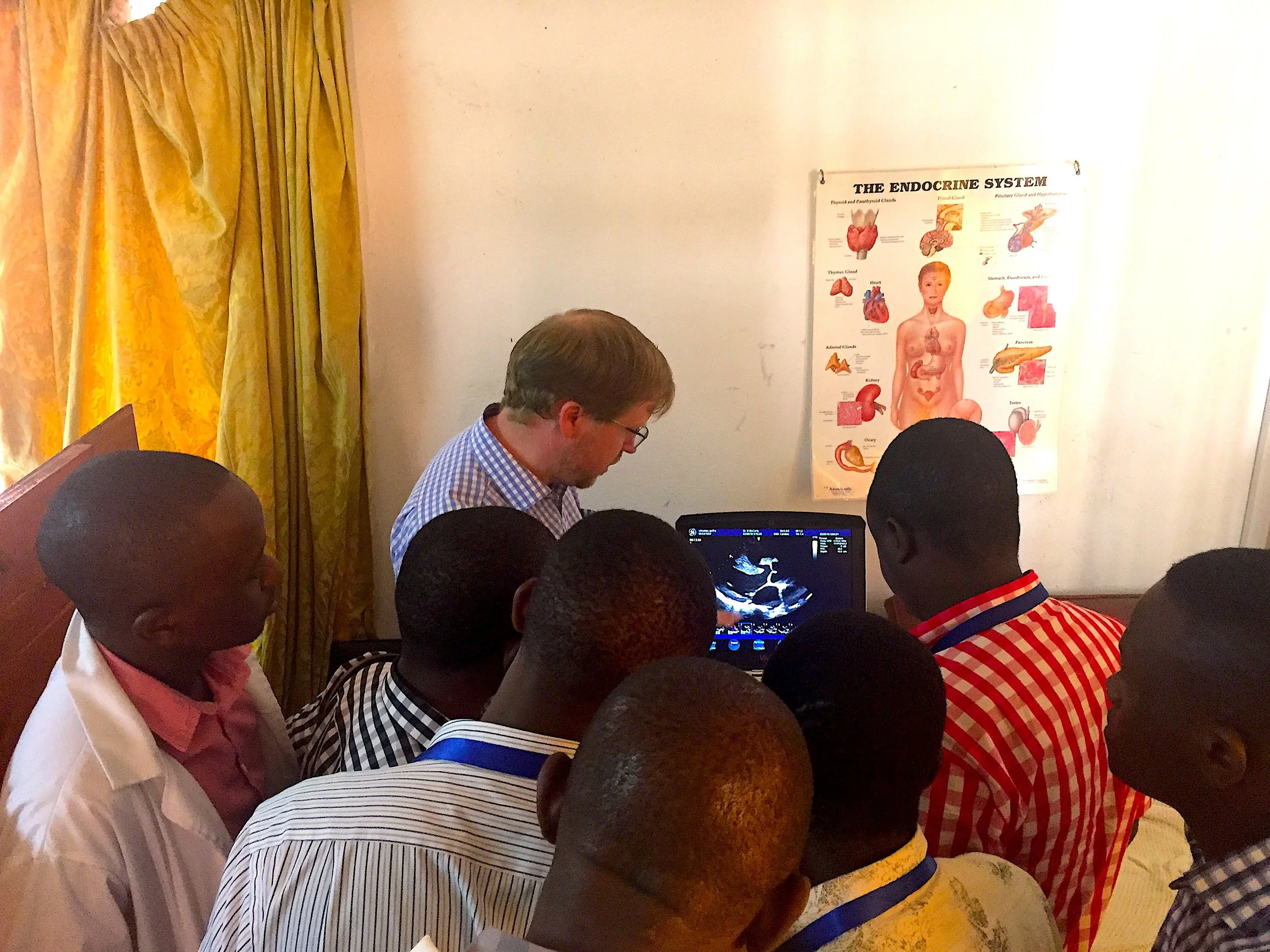
Point-Of-Care-Ultrasound (POCUS) demonstration
The method is deliberately unglamorous. Training is hands-on and standardized: apical four-chamber views, Doppler discipline, measurement reproducibility. Reporting templates are simple enough to use on a crowded ward round. Referral pathways are tightened so a borderline study doesn’t become a lost patient. Quality assurance is built in—peer review on tricky cases, feedback loops that fix technique before bad habits set. Technology matters, but only when it survives Tuesday: platforms are chosen for serviceability; data collection is designed for busy clinics, not glossy reports.
Blantyre concentrates both the challenges and the advantages of Malawi’s health system. Public care is free at the point of use, a principled promise that collides with stock-outs, staff gaps, and power cuts. Mission and private providers fill some of the space—sometimes with fees that keep the lights on and, just as often, keep patients away. In this context, the multiplier is competence. When a sonographer nails acquisition the first time, the queue shortens. When a clinical officer trusts the report, the referral is faster. When the ward moves, the hospital breathes.
Dr. McCarty teaching radiographers
Prevention and early detection run alongside capacity-building. MTIMA backs community education and pragmatic screening strategies because the best emergency is the one that never arrives. The work also tilts forward in time. Mentorship aims at students and early-career clinicians so today’s trainees become tomorrow’s service leads—without leaving Blantyre to learn what Blantyre needs.
None of this seeks to romanticize “The Warm Heart of Africa.” Warmth here is not sentiment; it’s infrastructure—the social trust that lets a clinic run on a bad day. Resolve isn’t loud; it’s daily—the habit of doing the next right thing whether the generator holds or not. By aligning with national priorities on non-communicable diseases and staying close to the realities of QECH wards and KUHeS classrooms, MTIMA keeps its footing where it counts: skills that stay, data that guide, systems that can take a punch.
Malawian Students’ First Ultrasound Exposure
Impact shows up in small, durable metrics that matter: fewer repeat scans because images are acquired correctly; cleaner reports that sharpen decisions; earlier interventions that send parents back to work and students back to class. These are not fireworks. They are fixtures. And in a city where exam rooms double as classrooms, fixtures are what last.
Blantyre is a useful lens for the wider story: a commercial hub with academic gravity, a place where policy meets bedside and where incremental improvements add up. The lesson is harder than it sounds and simpler than it looks. Build capacity you can measure. Center local leadership. Choose tools you can maintain. Then do it again tomorrow.
If you’re looking for transformation, it won’t arrive with a ribbon-cutting. It will look like a new habit of precision in a room that hums, a clinician who trusts the images on the screen, and a patient who leaves with a plan. That’s the headline MTIMA is after. And in Blantyre, it’s already in print.